Journal of Clinical and Biomedical Sciences
DOI: 10.58739/jcbs/v15i3.25.79
Year: 2025, Volume: 15, Issue: 3, Pages: 211-217
Original Article
Kumar D Ashwin1, Fathima Lubna2, Madugula Sowndarya3, Prabu D4∗, Rajmohan M5, Sindhu R2, Dinesh D5, Indira N2
1Undergraduate, Department of public health dentistry, SRM Dental college, Bharathi salai, Chennai, Tamil Nadu, India
2Senior lecturer, Department of public health dentistry, SRM Dental college, Bharathi salai, Chennai, Tamil Nadu, India
3Postgraduate, Department of public health dentistry, SRM Dental college, Bharathi salai, Chennai, Tamil Nadu, India
4Professor and Head, Department of public health dentistry, SRM Dental college, Bharathi salai, Chennai, Tamil Nadu, India
5Reader, Department of public health dentistry, SRM Dental college, Bharathi salai, Chennai, Tamil Nadu, India
*Corresponding Author
Email: [email protected]
Received Date:08 February 2025, Accepted Date:02 June 2025, Published Date:26 September 2025
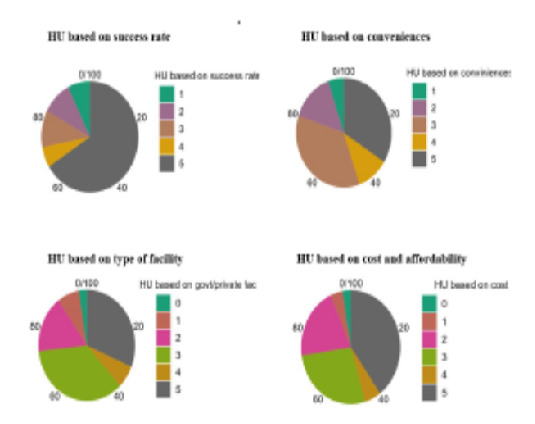
Background: Oral diseases pose a great burden across the world, especially among low to middle-income countries, owing to changes in dietary habits, urbanization, and individual economic constraints. Healthcare utilization (HU) plays an important role in lessening such burden. Individual perception of health status can provide insights to understand the problems with HU. Aim: The present study aims at understanding healthcare utility in individuals’ perspective among young adults of Chennai. Methods: 310 young adults were assessed Self-rated oral health status (SROH) and oral health related quality of life (OHRQoL) using oral health impact profile (OHIP-14). Total Healthcare utility (THU) was evaluated using standard gamble method. The association of gender, OHIP scores, and SROH with HU was assessed using Pearson’s Chi-square. Kruskal Wallis test was employed to compare the THU among participants grouped based on their frequency of dental visits. Results: Participants of mean age 23±8.96 reported good (80.6%), fair (12.6%), and poor (6.66%) oral health statuses. The mean HU score was 14.45±4.15. Significant associations were observed between OHIP and THU (P < 0.01), OHIP and HU based on convenience (P = 0.002), SROH and HU based on type of facility (P= 0.004), SROH and HU based on affordability (P = 0.041). A significant difference was found in THU scores among participants with different frequencies of dental visits (P = 0.001). Conclusion: The HU among young adults wasinfluenced by self-rated oral health status, OHRQoL, affordability, and type of healthcare facility. Consideration to HU was only given when there were perceived dental problems.
Graphic abstract
Keywords: Oral health impact profile; Self-rated oral health status; Affordability to healthcare; Dental visits; Health related quality of life
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Published By Sri Devaraj Urs Academy of Higher Education, Kolar, Karnataka
Subscribe now for latest articles and news.