Journal of Clinical and Biomedical Sciences
DOI: 10.58739/jcbs/v15i4.25.105
Year: 2025, Volume: 15, Issue: 4, Pages: 251- 256
Original Article
Ayesha Z Baig1, Vaijayanthi Kanabur2*
1PG Student, Department of Food and Nutrition, Smt. VHD Central Institute of Home Science, Maharani Cluster University, Bangalore- 560001, Karnataka, India.
2Associate Professor, Department of Food and Nutrition, Smt. VHD Central Institute of Home Science, Maharani Cluster University, Bangalore- 560001, Karnataka, India
*Corresponding Author
Email: [email protected]
Received Date:28 February 2025, Accepted Date:18 July 2025, Published Date:30 December 2025
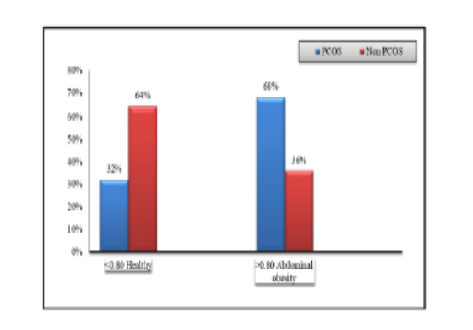
Background: An increasing number of women in the reproductive age are suffering from a hormonal disorder called Polycystic Ovarian Syndrome (PCOS). According to the World Health Organization (WHO 2023), PCOS affects an estimated 8 to 13 per cent of women of reproductive age worldwide. It is to be noted that nearly 70 per cent of this remains undiagnosed. PCOS is a complex condition characterized by increase in androgen levels, irregular menstrual cycle, and/or small cysts on one or both ovaries. In addition, psychological comorbidities are common in women with PCOS. Psychological factors may contribute to eating disorders and weight gain. There is a complex interrelationship between nutritional status and endocrine status. Research has shown that diet plays an important role in the regulation of metabolism of sex steroids and Luteinising Hormone (LH) secretions. Objective: To compare eating behaviour of women with and without PCOS. Materials and Methods: The study was conducted in selected areas of urban Bengaluru, Karnataka. The Three factor eating questionnaire (TFEQ), a revised 18 item tool developed by Karlsson Persson et al (2000) was used to assess the eating behaviour of the subjects. Women of age group 18-35 years suffering from PCOS (N=50) were compared with healthy women of the same age group (N=50). Results: The Body Mass Index (BMI) analysis shows that only 32 per cent of PCOS women had normal BMI compared to 48 per cent in case of Non-PCOS. It is observed that majority (68 per cent) of PCOS women have unhealthy Waist to Hip Ratio of >0.80. There was no difference in the dietary habits of the PCOS and Non-PCOS women. The eating behaviour analysed by three- factor eating indicated that emotional eating was highest in PCOS women, followed by uncontrolled eating and then cognitive eating. Conclusion: Binge eating, eating due to anxiety, depression and loneliness was more in women with PCOS as compared to control group.
Keywords: 18 item TFEQ; Eating disorder; Emotional eating; Uncontrolled eating; Cognitive eating
1. Umland EM, Weinstein LC, Buchanan EM. Menstruation-related disorders. Pharmacotherapy: A Pathophysiologic Approach. 8th ed. New York: McGraw-Hill; 2011. p. 139.
2. Naderi T, Akbarzadeh M, Manesh MHD, Tabatabaei H, Zareh Z. Frequency of facial and body acne in 14- to 18- year-old female high school students and its relationship to polycystic ovary syndrome. Journal of Dermatology and Cosmetic. 2011;2:124–131.
3. Varghese R, joy A, Saji SM, Radhakrishnan R. Health related complications associated with polycystic ovarian disease (PCOD). The Pharma Innovation Journal 2018;7(11):86–90.
4. Zehravi M, Maqbool M, Ara I. Polycystic ovary syndrome and infertility: an update. International Journal of Adolescent Medicine and Health. 2022; 34 (2). Available from: https://doi.org/10.1515/ijamh-2021-0073
5. Escobar-Morreale HF. Polycystic ovary syndrome: definition, aetiology, diagnosis and treatment. Nature Reviews Endocrinology. 2018; 14 (5). Available from: https://doi.org/10.1038/nrendo.2018.24
6. Dokras A, Clifton S, Futterweit W, Wild RA. Increased Risk for Abnormal Depression Scores in Women With Polycystic Ovary Syndrome. Obstetrics & Gynecology. 2011; 117 (1). Available from: https://doi.org/10.1097/aog.0b013e318202b0a4
7. Lee I, Cooney LG, Saini S, Smith ME, Sammel MD, Allison KC, et al. Increased risk of disordered eating in polycystic ovary syndrome. Fertility and Sterility. 2017; 107 (3). Available from: https://doi.org/10.1016/j.fertnstert.2016.12.014
8. Larsson I, Hulthén L, Landén M, Pålsson E, Janson P, Stener-Victorin E. Dietary intake, resting energy expenditure, and eating behavior in women with and without polycystic ovary syndrome. Clinical Nutrition. 2016; 35 (1). Available from: https://doi.org/10.1016/j.clnu.2015.02.006
9. Lalonde-Bester S, Mailk M, Masoumi R, Ng K, Sidhu S, Ghosh M. Prevalence and Etiology of Eating Disorders in Polycystic Ovary Syndrome: A Scoping Review. Advances in Nutrition. 2024; 15 (4). Available from: https://doi.org/10.1016/j.advnut.2024.100193
10. Teede HJ, Misso ML, Deeks AA, Moran LJ, Stuckey BGA, Wong JLA, et al. Assessment and management of polycystic ovary syndrome: summary of an evidence-based guideline. Medical Journal of Australia. 2011; 195 (6). Available from: https://doi.org/10.5694/mja11.10915
11. Stańczak NA, Grywalska E, Dudzińska E. The latest reports and treatment methods on polycystic ovary syndrome. Annals of Medicine. 2024; 56 (1). Available from: https://doi.org/10.1080/07853890.2024.2357737
12. Karlsson J, Persson LO, Sjöström L, Sullivan M. Psychometric properties and factor structure of the Three-Factor Eating Questionnaire (TFEQ) in obese men and women. Results from the Swedish Obese Subjects (SOS) study. International Journal of Obesity. 2000; 24 (12). Available from: https://doi.org/10.1038/sj.ijo.0801442
13. Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. Journal of Psychosomatic Research. 1985; 29 (1). Available from: https://doi.org/10.1016/0022-3999(85)90010-8
14. de Lauzon B, Romon M, Deschamps V, Lafay L, Borys JM, Karlsson J et al. The Three-Factor Eating Questionnaire-R18 Is Able to Distinguish among Different Eating Patterns in a General Population. The Journal of Nutrition. 2004; 134 (9). Available from: https://doi.org/10.1093/jn/134.9.2372
15. Anglé S, Engblom J, Eriksson T, Kautiainen S, Saha MT, Lindfors P, et al. Three factor eating questionnaire-R18 as a measure of cognitive restraint, uncontrolled eating and emotional eating in a sample of young Finnish females. International Journal of Behavioral Nutrition and Physical Activity. 2009; 6 (1). Available from: https://doi.org/10.1186/1479-5868-6-41
16. Hautala LA, Junnila J, Helenius H, Väänänen AM, Liuksila PR, Räihä H, et al. Towards understanding gender differences in disordered eating among adolescents. Journal of Clinical Nursing. 2008; 17 (13). Available from: https://doi.org/10.1111/j.1365-2702.2007.02143.x
17. Stefanaki K, Karagiannakis DS, Peppa M, Vryonidou A, Kalantaridou S, Goulis DG, et al. Food Cravings and Obesity in Women with Polycystic Ovary Syndrome: Pathophysiological and Therapeutic Considerations. Nutrients. 2024; 16 (7). Available from: https://doi.org/10.3390/nu16071049
18. Jeanes YM, Reeves S, Gibson EL, Piggott C, May VA, Hart KH. Binge eating behaviours and food cravings in women with Polycystic Ovary Syndrome. Appetite. 2017; 109 Available from: https://doi.org/10.1016/j.appet.2016.11.010
19. Hart K, Evil R, Clavert A, Hodgson J, Gibson EL, Jeanes Y. Eating behaviours in women with polycystic ovary syndrome and healthy comparators. Journal of Human Nutrition and Dietetics. 2012;25(6):604.
20. Lydecker JA, Grilo CM. Comparing men and women with binge‐eating disorder and co‐morbid obesity. International Journal of Eating Disorders. 2018; 51 (5). Available from: https://doi.org/10.1002/eat.22847
21. Moroshko I, Brennan L, O’Brien P. Predictors of dropout in weight loss interventions: a systematic review of the literature. Obesity Reviews. 2011; 12 (11). Available from: https://doi.org/10.1111/j.1467-789x.2011.00915.x
22. Grucza RA, Przybeck TR, Cloninger CR. Prevalence and correlates of binge eating disorder in a community sample. Comprehensive Psychiatry. 2007; 48 (2). Available from: https://doi.org/10.1016/j.comppsych.2006.08.002
23. Jeanes YM, Reeves S, Gibson EL, Piggott C, May VA, Hart KH. Binge eating behaviours and food cravings in women with Polycystic Ovary Syndrome. Appetite. 2017; 109 Available from: https://doi.org/10.1016/j.appet.2016.11.010
24. Pesonen E, Nurkkala M, Ollila MM, Hurskainen E, Morin-Papunen LC, Jämsä T, et al. Women with polycystic ovary syndrome are at risk of emotional and uncontrolled eating at midlife: a population-based cohort study. Fertility and Sterility. 2025; 123 (3). Available from: https://doi.org/10.1016/j.fertnstert.2024.09.042
25. Sharma S, Lata G, Manchanda S, Kaur S. Prevalence of Anxiety, Depression and Eating Disorders in Women with Polycystic Ovarian Syndrome in North Indian Population of Haryana. Galore International Journal of Health Sciences and Research. 2019 4(4). 61-67.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Published By Sri Devaraj Urs Academy of Higher Education, Kolar, Karnataka
Subscribe now for latest articles and news.