Journal of Clinical and Biomedical Sciences
DOI: 10.58739/jcbs/v15i4.25.133
Year: 2025, Volume: 15, Issue: 4, Pages: 268-276
Original Article
Avinash Kumar1*, Sangeeta Datta2, Biswaroop Chatterjee3
1Associate Professor, Department of Microbiology, IQ City Medical College and Hospital, Durgapur-713206, West Bengal, India.
2Junior Resident, Department of Microbiology, IQ City Medical College and Hospital, Durgapur-713206, West Bengal, India.
3Professor, Department of Microbiology, IQ City Medical College and Hospital, Durgapur-713206, West Bengal, India.
*Corresponding Author
Email: [email protected]
Received Date:22 July 2025, Accepted Date:14 November 2025, Published Date:31 December 2025
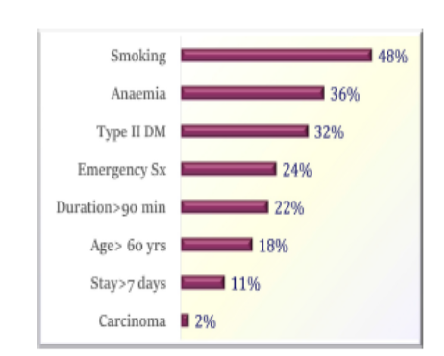
Background: Surgical site infections (SSI) are estimated to be the most prevalent type of healthcare-associated infections, continuing to pose a significant source of morbidity, economic burden, and mortality. Aim: This study aims to estimate the burden of SSI across various surgical specialties, risk factors, distribution of predominant pathogens, and their antibiogram at a tertiary-care hospital in Eastern India. Methodology: This was a descriptive, cross-sectional study conducted over a period of 24 months, from January 2023 to February 2025. All SSI cases were included according to guidelines from the Centers for Disease Control and Prevention. Samples were collected, and organisms were identified and tested for antimicrobial susceptibility using the MicroScan WalkAway® plus system (Beckman Coulter, California, USA). SSI rates were calculated by dividing the number of SSIs by the number of operative procedures and multiplying the result by 100. Results: Of total 6,628 surgeries, 358 cases were identified as SSI, resulting in a rate of 5.4%, with the majority occurring in the orthopaedics department. Smoking, anaemia, and diabetes mellitus were the most prevalent risk factors. Growth was observed in 87%, with Staphylococcus aureus and Escherichia coli being the predominant pathogens. Methicillin-resistant Staphylococcus aureus (MRSA) accounted for 45%, and Vancomycin-resistant Enterococcus (VRE) was 20%. Among the Enterobacterales, 70% of Klebsiella spp., 44% of Escherichia coli, and 32% of Proteus spp. were identified as multidrug-resistant (MDR). All isolates of Acinetobacter calcoaceticus-baumannii complex and 35% of Pseudomonas aeruginosa were identified as MDR. Conclusion: The high SSI rates in different departments underscore the need for improved infection control practices and the establishment of a robust antimicrobial stewardship program. Surveillance of SSI cases, along with feedback, and regular auditing of prophylaxis protocols and resistance trends, is essential to reduce their prevalence.
Keywords: Surgical site infections; Antimicrobial resistance; Multidrug-resistant; Methicillin-resistant <I>Staphylococcus aureus</I>; Vancomycin-resistant <I>Enterococcus</I>
1. World Health Organization. Global Guidelines for the prevention of surgical site infection. WHO Guidelines Development Group; Geneva, Switzerland. 2016:58–177. Available from https://www.who.int/publications/i/item/9789241550475
2. Centers for Disease Control and Prevention. Surgical Site Infection (SSI) Events; 2025. Available from https://www.cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.pdf
3. Mekhla, Borle FR. Determinants of superficial surgical site infections in abdominal surgeries at a Rural Teaching Hospital in Central India: A prospective study. Journal of Family Medicine and Primary Care. 2019; 8 (7). Available from: https://doi.org/10.4103/jfmpc.jfmpc_419_19
4. Gupta BB, Soman K, Bhoir L, Gadahire M, Patel B, Ahdal J. The Burden of Methicillin Resistant <I>Staphylococcus aureus</I> in Surgical Site Infections: A Review. Journal of Clinical and Diagnostic Research. 2021; 15 (5). Available from: https://doi.org/10.7860/jcdr/2021/46922.14891
5. Deka S, Kalita D, Mahanta P, Baruah D. High Prevalence of Antibiotic-Resistant Gram-Negative Bacteria Causing Surgical Site Infection in a Tertiary Care Hospital of Northeast India. Cureus. 2020; 12 (12). Available from: https://doi.org/10.7759/cureus.12208
6. Cui P, Fang X. Pathogenesis of infection in surgical patients. Current Opinion in Critical Care. 2015; 21 (4). Available from: https://doi.org/10.1097/mcc.0000000000000227
7. Tamma PD, Heil EL, Justo JA, Mathers AJ, Satlin MJ, Bonomo RA. Infectious Diseases Society of America 2024 Guidance on the Treatment of Antimicrobial-Resistant Gram-Negative Infections. Clinical Infectious Diseases. 2024; Available from: https://doi.org/10.1093/cid/ciae403
8. Hirani S, Trivedi NA, Chauhan J, Chauhan Y. A study of clinical and economic burden of surgical site infection in patients undergoing caesarian section at a tertiary care teaching hospital in India. PLoS One. 2022; 17 (6). Available from: https://doi.org/10.1371/journal.pone.0269530
9. Karan K, Kulkarni SR, Gayatri, Tripathi SV, Puppal AN. Surgical Site Infection in Clean, Clean-Contaminated and Contaminated Cases. Journal of Medical Science And clinical Research. 2016; 04 (12). Available from: https://doi.org/10.18535/jmscr/v4i12.111
10. Mohan N, Gnanasekar D, Tk S, Ignatious A. Prevalence and Risk Factors of Surgical Site Infections in a Teaching Medical College in the Trichy District of India. Cureus. 2023; 15 (5). Available from: https://doi.org/10.7759/cureus.39465
11. Negi V, Pal S, Juyal D, Sharma MK, Sharma N. Bacteriological Profile of Surgical Site Infections and Their Antibiogram: A Study From Resource Constrained Rural Setting of Uttarakhand State, India. Journal of Clinical and Diagnostic Research. 2015; 9 (10). Available from: https://doi.org/10.7860/jcdr/2015/15342.6698
12. Verma U, Ashopa V, Gupta E, Gupta A, Lal P, Gupta PC, <I>et al</I>. Bacteriological Profile of Surgical Site Infection in a Tertiary Care Centre. International Journal of Current Microbiology and Applied Sciences. 2021; 10 (3). Available from: https://doi.org/10.20546/ijcmas.2021.1003.267
13. Banik A, Haldar S, Kundu S, Bhunia S, Behera KK, Roy C, <I>et al</I>. A study on clinico-demographic and microbiological profile of surgical site infection (SSI) in a tertiary care hospital, Kolkata: An alarming trend. Indian Journal of Microbiology Research. 2024; 11 (1). Available from: https://doi.org/10.18231/j.ijmr.2024.005
14. Chada CKR, Kandati J, Ponugoti M. A prospective study of surgical site infections in a tertiary care hospital. International Surgery Journal. 2017; 4 (6). Available from: https://doi.org/10.18203/2349-2902.isj20172109
15. Choudhury K, Basu S, Bhattacharjee SG, Sikdar S, Deb S, Tabassum N. Surgical site infection: Clinico- bacteriological Profile and antibiogram in a tertiary care hospital in Kolkata. Panacea Journal of Medical Sciences. 2023; 13 (2). Available from: https://doi.org/10.18231/j.pjms.2023.058
16. Kasukurthy LR, Bathala M. Bacteriological Profile of Surgical Site Infections (SSIs)- A Study in a Tertiary Care Hospital. Journal of Evidence Based Medicine and Healthcare. 2020; 7 (32). Available from: https://doi.org/10.18410/jebmh/2020/338
17. Khan AS, Sarwat T, Mohan S, Dutta R. Surgical Site Infection: Bacteriological and Clinicopathological Profile and Antibiogram in a Tertiary Care Hospital. Journal of Medical Sciences and Health. 2021; 6 (3). Available from: https://doi.org/10.46347/jmsh.2020.v06i03.009
18. Pham JC, Ashton MJ, Kimata C, Lin DM, Nakamoto BK. Surgical site infection: comparing surgeon versus patient self-report. Journal of Surgical Research. 2016; 202 (1). Available from: https://doi.org/10.1016/j.jss.2015.12.039
19. Kumar A, Rai A. Prevalence of surgical site infection in general surgery in a tertiary care centre in India. International Surgery Journal. 2017; 4 (9). Available from: https://doi.org/10.18203/2349-2902.isj20173896
20. Dhote N, Nagdeo N. Bacteriological profile of surgical site infection and associated risk factors in obstetrics and Gynecology patient. Panacea Journal of Medical Sciences. 2018; 8 (2). Available from: https://doi.org/10.18231/2348-7682.2018.0016
21. Pradeep MSS, Rao KVV. A Study on surgical Site Infections, their bacteriological profile and antimicrobial susceptibility pattern. IP International Journal of Medical Microbiology and Tropical Diseases. 2019; 5 (1). Available from: https://doi.org/10.18231/2581-4761.2019.0003
22. Kokate SB, Rahangdale V, Katkar VJ. Study of Bacteriological Profile of Post Operative Wound Infections in Surgical Wards in a Tertiary Care Hospital. IJCMR. 2017; 4 (1). Available from: https://doi.org/10.70284/njirm.v9i2.2309
23. Deb S, Sarkar S, Chatterjee C, Pal NK, Ganguly S. Study of gram negative non fermenting bacilli from surgical site infections in a tertiary care hospital in Kolkata. <I>International Journal of Research and Review</I>. 2019;6(7):169–74.
24. Patnaik N, Mallick B, Kar A. Aerobic Bacteriological Profile of Surgical Site Infection with Special Reference to MRSA at Hitech Medical College and Hospital, Bhubaneswar. International Journal of Current Microbiology and Applied Sciences. 2019; 8 (02). Available from: https://doi.org/10.20546/ijcmas.2019.802.036
25. Aghdassi SJS, Gastmeier P, Hoffmann P, Schwab F. Increase in surgical site infections caused by gram-negative bacteria in warmer temperatures: Results from a retrospective observational study. Infection Control & Hospital Epidemiology. 2021; 42 (4). Available from: https://doi.org/10.1017/ice.2020.463
26. Zamel HA. Surgical Site Infection Surveillance. <I>Infection Control Today</I>. 2023;27(5).
27. Gurunthalingam MP, Keche YN, Gaikwad NR, Dhaneria S, Singh MP. Appropriateness of Surgical Antibiotic Prophylaxis in a Tertiary Care Teaching Hospital in Central India: A Retrospective Analysis. Cureus. 2023; 15 (5). Available from: https://doi.org/10.7759/cureus.38844
28. World Health Organization. Global Antimicrobial Resistance and Use Surveillance System (GLASS) Report: 2022. Geneva, Switzerland. 2022. Available from: https://www.who.int/pubLications/i/item/9789240062702
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Published By Sri Devaraj Urs Academy of Higher Education, Kolar, Karnataka
Subscribe now for latest articles and news.